Non-Alcoholic Fatty Liver Disease (NAFLD) is a growing health concern that has risen rapidly in parallel to the increasing weight of the population. Nutritional supplements have emerged as a supportive tool for people with fatty liver disease. While they are not a cure-all, certain supplements can complement diet and lifestyle changes in managing NAFLD. This article explores how specific supplements, such as Omega-3 fatty acids, Vitamin E, and milk thistle, among others, can support liver health.
Along with providing information on which NAFLD supplements might be right for you, this article also links to Fullscript where you can buy these liver support supplements online through the secure healthcare formulary and get free shipping and 20% off the retail price of professional-grade supplements.
We explore the research behind each supplement and show how they can contribute to improved liver function, reduce inflammation, and assist in managing this increasingly common liver condition.
What Is NAFLD?
NAFLD was recently renamed to remove any stigma associated with alcohol. It will now be metabolic dysfunction-associated steatotic liver disease (MASLD). MASLD encompasses patients who have hepatic steatosis and have at least one of five cardiometabolic risk factors.
NAFLD/MASLD is a common condition characterized by the accumulation of excess fat in liver cells in individuals who consume little or no alcohol. It’s becoming increasingly common, partly due to rising obesity rates worldwide. NAFLD is often silent, with few or no symptoms, especially in the early stages. When symptoms do appear, they may include fatigue, pain or discomfort in the upper right abdomen, and sometimes swelling in the abdomen.
NAFLD/MASLD is primarily caused by a combination of lifestyle factors and genetics. The main risk factors include obesity, insulin resistance, type 2 diabetes, and high levels of fats, particularly triglycerides, in the blood. Poor eating habits, a sedentary lifestyle, and excessive calorie intake also contribute to its development.
While NAFLD/MASLD can be benign and not progress, it can sometimes evolve into a more serious condition known as non-alcoholic steatohepatitis (NASH), which involves inflammation and damage to liver cells, potentially leading to cirrhosis or liver cancer. Early detection and lifestyle modifications play a crucial role in managing NAFLD/MASLD and preventing its progression.
What Food and Lifestyle Factors Are Important For Managing Fatty Liver?
Managing Non-Alcoholic Fatty Liver Disease (NAFLD) effectively centers on weight loss. When a person loses weight, it directly reduces fat in the liver and decreases inflammation. Losing even a modest amount of weight can greatly improve liver health and function. Regular physical activity, such as brisk walking, cycling, or swimming, not only helps with weight loss but also improves overall liver function. Getting enough quality sleep is critical for weight management, as it helps regulate metabolism. Managing stress through techniques like yoga, meditation, or deep breathing is also important because chronic stress can lead to weight gain and worsen NAFLD.
Diet plays a critical role too. Avoiding alcohol is essential, as it can worsen liver damage. Sugary beverages, especially sodas with high fructose corn syrup can be very damaging to the liver by causing liver fat accumulation and causing further liver injury. By focusing on long-term weight management and dietary factors, people can greatly influence the progression of NAFLD.
Some studies have shown that coffee may have liver-protective effects and could be beneficial in managing NAFLD. [PMID: 27824642]
What Nutritional Supplements Are Recommended For NAFLD/MASLD ?
- Omega-3 Fatty Acids: These fatty acids, found in fish oil, are effective in reducing liver fat and inflammation in NAFLD by modifying fat metabolism and suppressing pro-inflammatory processes in the liver. [PMC7551292]
- Milk Thistle (Silymarin): Milk thistle aids in reducing liver inflammation and damage due to its antioxidant properties, which help protect liver cells from toxins and support liver regeneration in NAFLD. [PMC9149185][PMC5728929]
- Multivitamin: [PMC9511103]
- Zinc: Zinc plays a critical role in liver health, and its supplementation can help in reducing liver damage in NAFLD by supporting antioxidant defense systems and improving immune function in the liver.
- Vitamin E: Acting as an antioxidant, Vitamin E helps in improving liver function in NAFLD by protecting liver cells from oxidative stress and may slow the progression of liver fibrosis, especially beneficial for those without diabetes.
- Selenium: As an antioxidant, selenium might help reduce oxidative stress and liver inflammation associated with NAFLD.
- Vitamin D: Some studies suggest that Vitamin D supplementation might improve liver health in NAFLD, especially since Vitamin D deficiency is common in individuals with this condition.
- B-Complex Vitamins: B vitamins, particularly B12 and folate, can support overall liver health and may aid in managing NAFLD, especially since some individuals with liver disease are deficient in these vitamins.
- Magnesium: A 16-week study found that L-carnitine (2 gr) combined with magnesium (150 mg) supplementation led to a reduction in liver enzymes, insulin levels, lipid profile, and liver stiffness.
- Curcumin: Found in turmeric, curcumin is known for its anti-inflammatory and antioxidant properties. It may help reduce liver inflammation and oxidative stress in NAFLD. [PMID: 33861434]
- Berberine: This compound, found in several plants, is believed to improve insulin resistance and reduce fat buildup in the liver, which can be beneficial in NAFLD. [PMC4947506]
- Green Tea Extract: Rich in antioxidants, particularly catechins, green tea extract may help reduce liver fat accumulation and inflammation in NAFLD. [ PMC8949532]
- L-Carnitine: This supplement may help reduce liver fat and improve liver function in NAFLD by helping in the metabolism of fatty acids. [PMC10148537]
- Taurine: This amino acid is believed to have hepatoprotective effects, potentially reducing liver inflammation and oxidative stress in humans [PMID: 36314323] and animal models of NAFLD. [PMID: 21126079]
- Coenzyme Q10 (CoQ10): Known for its antioxidant properties, CoQ10 may help reduce oxidative stress in the liver, which is beneficial for NAFLD management. [PMC10261764]
- Probiotics: The intestinal flora is closely related to the pathogenesis of nonalcoholic fatty liver disease (NAFLD). These beneficial bacteria enhance liver function in NAFLD patients by restoring balance to the gut microbiome, which can positively impact liver health by reducing gut-derived toxins and inflammation. [PMC9875992]
Dietary supplements are not designed to diagnose, treat, cure, or prevent any disease. This article aims to offer valuable insights into which nutritional supplements have undergone scientific study and shown promise in supporting specific health conditions. We break down the research, so you can work with your medical providers to make informed decisions about adding supplements to your health regimen. For personalized advice tailored to your needs, we recommend consulting with a registered dietitian in addition to your primary care provider.
Check with your physician when adding supplements. While supplements are generally safe for most people, do not add nutritional supplements without your physician’s specific approval if you are pregnant or nursing, are undergoing cancer treatment, have a history of organ transplant, liver or kidney disease, or take medications that interact with supplements.
Order Supplements For Managing Fatty Liver
Why Professionals Choose the Fullscript Formulary
Your health is on the line. Health professionals know that many other online and retail options set a very low bar for quality–sometimes amazingly low. The Fullscript formulary is the most secure online source for the highest quality brands securely sourced to assure freshness and purity. Here’s what makes Fullscript the best:
- Meticulous vetting of brand quality. Health professionals trust Fullscript to continuously monitor the quality of each item on the platform. Other retailers operate with profit as their highest or only motive when choosing brands. Fullscript cares only about quality and reliability. Unlike discount stores, large online marketplaces, and other retailers you won’t find ingredients sourced from China or other questionable locations or companies.
- Always 20% Discount off the manufacturer’s retail price. When you follow any link from Supplement-Sciences.com, you will automatically get 20% off the retail price.
- Free shipping over $50.
- Freshness. Fullscript prioritizes freshness over bulk buying even if it means an increased risk of briefly being out of stock.
- Top quality phone and online support. When you call, knowledgeable humans at Fullscript answer your questions.
- How It Works:
- Easy Sign-up & No Spam Email: Click the “View Product” button below to be taken to Fullscript’s login page where you can quickly create your secure account with just your name, email, and phone number. Then you will be taken directly to the product page.
- Wide variety of supplement options: Once you sign in to your account, you are not limited to the products listed below. You will see similar items listed at the bottom of each product page on Fullscript.
- Search For What You Want: Once inside Fullscript, you can search for the exact brands and products you want from their wide selection of quality brands.

When you purchase linked products presented on this page, Supplement Sciences, LLC receives affiliate fees so that our dietitians can continue to create great content.
Thank you for your support!
Are Supplements Safe?
Omega-3 Fatty Acids, Multivitamins, Milk Thistle (Silymarin), Probiotics, Curcumin, Berberine, N-Acetyl Cysteine (NAC), Alpha-Lipoic Acid, Green Tea Extract, Resveratrol, Vitamin D, L-Carnitine, Taurine, B-Complex Vitamins, Coenzyme Q10 (CoQ10), and Dandelion Root are generally safe for use in the context of managing Non-Alcoholic Fatty Liver Disease (NAFLD)/Metabolic Associated Fatty Liver Disease (MAFLD). When used in recommended dosages and under medical guidance, these supplements are known to be well-tolerated with minimal side effects. It’s important to note that they are not substitutes for medical treatment but can be used as part of a broader health management plan.
Medication Interactions:
- Blood Thinners (Anticoagulants): Omega-3 Fatty Acids can enhance the blood-thinning effect and increase bleeding risk, while Green Tea Extract, containing vitamin K, can counteract the effects of blood thinners, and Ginkgo Biloba is known to increase the risk of bleeding.
- Diabetes Medications: Berberine and Alpha-Lipoic Acid can both lower blood sugar, possibly requiring adjustments in diabetes medication, and Ginseng can also affect blood sugar levels and interact with diabetes medications.
- Blood Pressure Medications: Licorice Root can elevate blood pressure and interfere with these medications, and Omega-3 Fatty Acids can potentially lower blood pressure, enhancing the effects of these drugs.
- Immunosuppressants: Echinacea can stimulate the immune system and may interfere with the action of immunosuppressants, and Astragalus might counteract the effects of these medications. Probiotics also interact with the immune system by affecting gut health.
- Chemotherapy Drugs: Green Tea Extract’s antioxidants can potentially interfere with the effectiveness of certain chemotherapy drugs, and Turmeric/Curcumin can interfere with the metabolism of some chemotherapy drugs.
- Statins (Cholesterol-Lowering Medications): Coenzyme Q10 (CoQ10) levels can be reduced by statins, and Niacin (Vitamin B3), when taken with statins, can increase the risk of muscle pain and damage.
It’s important to consult with a healthcare professional because interactions can vary based on individual health conditions and medication dosages.
Supplement Interactions:
- Omega-3 Fatty Acids: May increase the risk of bleeding when taken with supplements that have blood-thinning properties, like Ginkgo biloba or high-dose vitamin E.
- Milk Thistle (Silymarin): May change the effectiveness of supplements metabolized by the liver, such as Glucosamine.
- Curcumin: May enhance the blood-thinning effects of supplements like Omega-3 fatty acids or vitamin E.
- Berberine: Can interact with supplements that lower blood sugar levels, like cinnamon, potentially leading to hypoglycemia.
- N-Acetyl Cysteine (NAC): May interact with nitrate supplements, affecting blood vessel dilation.
- Alpha-Lipoic Acid: Can lower blood sugar levels and may interact with other supplements that have similar effects.
- Green Tea Extract: Contains caffeine and can interact with other stimulant supplements, possibly leading to increased heart rate and blood pressure.
- Resveratrol: May enhance the blood-thinning effects of supplements like Omega-3 fatty acids or vitamin E.
- L-Carnitine: Can interact with anticoagulant supplements, potentially enhancing their effects.
- Coenzyme Q10 (CoQ10): Statins can reduce CoQ10 levels in the body, and CoQ10 supplements can interact with blood-thinning supplements, affecting their efficacy.
The Fasting Mimicking Diet For Fatty Liver
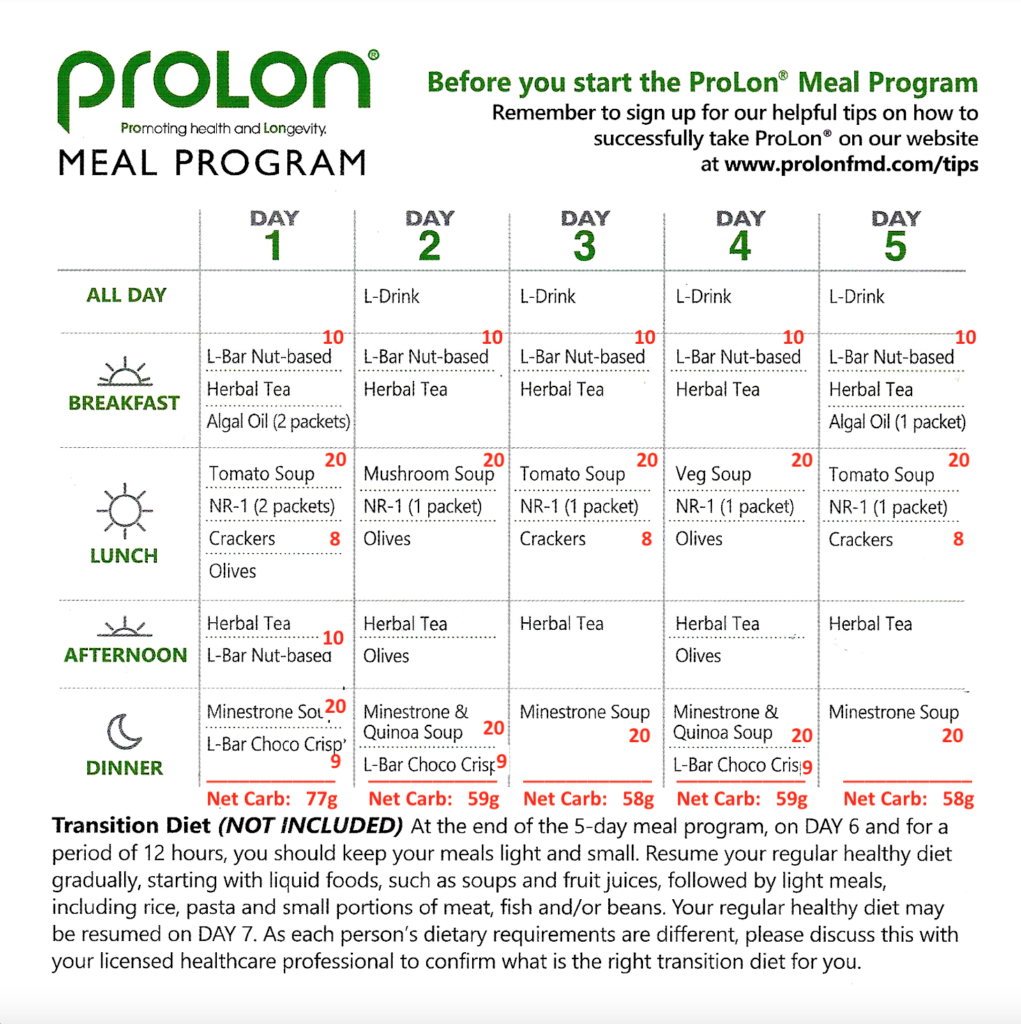
Intermittent fasting is shown to improve liver function markers and promote weight loss in adults with fatty liver. [PMC10552959, PMID: 36343094]. An alternative option is the “fasting mimicking diet”, a 5 day low calorie, low protein, high nutrient density diet. Read more in our full article: ProLon: The Easy Way To Get the Benefits of Fasting.
The fasting-mimicking diet (FMD) mimics the effects of traditional fasting while still providing essential nutrients.The FMD state encourages the body to use up stored fats, which can directly help in reducing liver fat accumulation and promotes the removal of damaged cells and tissues, a process known as autophagy, which can improve liver function and reduce inflammation. By periodically implementing FMD, it helps in resetting the body’s metabolic processes, which is crucial in managing conditions like NAFLD where metabolism is significantly disrupted. This approach, therefore, offers a strategic and manageable way to address the underlying causes of NAFLD, improving liver health and overall metabolic function. [PMC6816332]
A recent study in a mouse model of fatty liver disease explored whether a fasting-mimicking diet (FMD), which involves intermittent calorie restriction, could help manage NAFLD. This special diet is low in carbohydrates and protein but high in dietary fibers. Not only did the diet help reduce obesity and improve blood sugar control, but it reduced the buildup of fat in the liver and decreased signs of liver inflammation. Additionally, gene analysis showed that the diet increased the liver’s ability to break down fats. Researchers concluded that intermittent use of the FMD can be effective in improving NAFLD. It works by enhancing the breakdown of fats in body fat and boosting the liver’s capacity to process and get rid of fats. Researchers concluded that FMD could be a promising approach for managing fatty liver disease. [PMID: 34632700]
Order Prolon FMD Kits Through Fullscript
Gen3 Prolon Kit by ProLon
ProLon® is a 5-day dietary program carefully designed to nourish and rejuvenate your body while supporting metabolic balance.*
The ProLon FastingMimicking Diet® gives many of the benefits of a fast while letting you eat delicious food to help fight hunger and lose weight while protecting lean body mass. Get a trimmer waistline and many of the associated benefits.*
ProLon® meals come in 5 small boxes (one for each day) that include plant-based energy bars, soups, a variety of snacks, drinks, and supplements, and carefully designed to nourish your body, support cellular rejuvenation, and support metabolic and overall health for healthy aging.*
With ProLon, you get everything you need pre-packaged and ready to go. Each kit comes with five boxes which are labeled by day so you know what to eat each day.
-GEN3 Soup Flavors: Red Bell Pepper & Onion, Green Pea & Chives, Lentil Curry, Chickpea & Leeks, Carrot Ginger
-Soups: A variety of easy-to-prepare soups made with a proprietary mix of all-natural, plant-based ingredients
-Nut Bars: Cold-pressed, delicious nut bars with whole ingredients like almonds, macadamia nuts, and pecans
-Snacks: Snacks like olives from the South of Spain where olive consumption is associated with longevity, and kale crackers enriched with plant-based protein.
-Supplements: Dietary supplement packed with multivitamins, amino-acids, minerals and omega-3 fatty acid to provide the body with nourishment
-L-Drink: Fruit-flavored, proprietary glycerol mix designed to fuel and protect muscles throughout the fast
-Herbal Teas: Caffeine-free herbal teas loaded with healthy antioxidants, and will keep you hydrated during your week.
Gen1 Prolon Kit by ProLon
Gen1 Prolon Kit, is a plant-based, 5-day meal program providing 1150 calories on Day 1 and approximately 800 on Days 2-5.
ProLon® exploits the ability of the body during periods of low calorie intake to enter a protected mode, remove damaged cells and tissues, and undergo self-repair.*
The ProLon® meal program consists of proprietary plant-based soups, bars, drinks, snacks, teas, and supplement formula tablets – all designed to maximize the protective effects related to fasting, while providing micronutrient nourishment (vitamins, minerals and essential dietary components), and minimizing hunger and the burdens of fasting.* The program covers a period of 5 continuous days.*
Order FMD Kits Directly Through The Prolon Site
Prolon 5-Day Fasting Mimicking Diet Kit
This kit contains 1 box of food for each day of the 5-day fast. Nutrients in each food kit are carefully calculated to keep nutrients at a level that will trigger the body’s cellular machinery to go into fasting mode as though you were eating nothing at all.
Foods are all vegan, gluten-free, and taste delicious.
Food First!
Although this article discusses supplements in detail, don’t forget that we are absolutely committed to the “Food First” approach to nutrition. When it comes to your health, the totality of your eating habits far surpasses the impact of individual nutrients or any single supplement you consume. Even though this article doesn’t delve into the broader picture of your overall diet, it’s crucial to keep this element at the forefront of our minds. Your food needs to provide all the vitamins, minerals, fiber, and phytochemicals to nourish your body systems down to the cellular level.
Food choices, rather than supplements, are the most critical factors for a healthy gut microbiome. These trillions of tiny inhabitants in your gut affect your brain waves; they orchestrate your immune system. They possess the power to create molecules that can switch genes on or off and are even capable of synthesizing neurotransmitters. Opting for organic foods and steering clear of plastic packaging (including those labeled BPA-free) is a smart move to limit toxin exposure. The sum of all these parts leads to a powerful conclusion: the ultimate key to your health lies in the quality and balance of the food you consume. Supplements are secondary.
What Lab Tests Might Be Helpful In Managing NAFLD/MASLD ?
Liver Function Tests (LFTs) and blood sugar tests, including Hemoglobin A1c (HbA1c), are really important for understanding and managing fatty liver disease. LFTs check for certain enzymes in your liver, mainly ALT and AST. If these are high, it could mean there’s some inflammation or damage in your liver, which often happens with NAFLD. By regularly checking these enzymes, doctors can see how the disease is progressing and whether the treatments are working.
Then there are blood sugar tests, including fasting glucose and HbA1c. These are important because NAFLD is often linked to problems with blood sugar control, like in diabetes or metabolic syndrome. Basically, these tests show how well your body is managing its blood sugar levels. For people with NAFLD, keeping an eye on blood sugar is crucial because problems with blood sugar control can make the liver condition worse.
To Sum It Up
A wide array of supplements have been researched for their benefit in fatty liver disease. The best results have been found with Omega-3 Fatty Acids, Multivitamins, Milk Thistle, Probiotics, Curcumin, Berberine, N-Acetyl Cysteine, Alpha-Lipoic Acid, Green Tea Extract, Resveratrol, Vitamin D, L-Carnitine, Taurine, and Coenzyme Q10. Although it might not be financially feasible to supplement with all of these, they each provide benefit.
Each of these supplements brings unique properties to the table, ranging from anti-inflammatory and antioxidant effects to liver support and metabolic health improvements. While these supplements can be beneficial, it’s crucial to remember that they should complement, not replace, traditional medical treatments and a healthy lifestyle. One of the most critical issues in fatty liver disease in weight loss. A dietitian can offer personalized counseling in this area that can help a person avoid the diet roller coaster and manage their weight with a long-term, health focused approach.
This Article is Not a Substitute for Medical Advice
Dietary supplements are not designed to diagnose, treat, cure, or prevent any disease. The Supplement Sciences website seeks to provide comprehensive access to the most relevant supplement information along with convenient online ordering. We do not provide medical advice and cannot guarantee that every product suggested is completely without risk. Since each person is unique in their health history and medication use, it is important to discuss supplements with your personal physician. Specifically, pregnant women and individuals being treated for cancer or liver or kidney problems must consult their physician about every nutritional supplement they plan to take. People taking medications for the treatment of HIV or with a history of organ transplant must not take supplements without consulting with their physician.

 Scan Me!
Scan Me!


