
Secure Ordering | Free Shipping | 20% Off Retail Prices
Here’s a discussion of the root causes of digestive problems and how they can be distinguished from one another. Along with this, we’ll suggest a few supplements for digestion that are likely to provide some relief. If you decide these digestive supplements might be right for you, this article also links to Fullscript where you can buy supplements for digestion online through the secure healthcare formulary and get free shipping and 20% off the retail price of professional-grade supplements.
Digestive problems can be a mild discomfort or debilitating conditions. They present a complex challenge in both understanding and treatment. The root causes of these issues are as diverse as the symptoms they produce, often making diagnosis a challenging endeavor. From food habits and lifestyle factors to infections, genetic predispositions, and chronic diseases, The array of potential triggers includes food habits and lifestyle factors, infections, genetic predispositions, and chronic diseases. Symptoms overlap greatly.
In this article, we take a deep dive into the various underlying causes of digestive disorders. We explore how they manifest and the diagnostic tools and techniques used to identify them. By shedding light on the intricacies of gastrointestinal health, we aim to provide a clearer path for those seeking answers and relief from digestive ailments.
What Are The Root Causes of Digestive Problems?
Food Habits: The connection between diet and digestive health is well-established. Fatty meats and fried foods, because they are high in fat, can slow down the digestive process. This makes it harder for the stomach to empty and leads to discomfort and heartburn. Sugary and highly processed foods can change the balance of bacteria in the gut. Sugar leads to dysbiosis, a condition where harmful bacteria outnumber beneficial ones, causing gas, bloating, and diarrhea. On the other hand, a diet lacking in fiber can lead to constipation. Fiber is needed for adding bulk and softness to stools, ensuring regular bowel movements. Many people are lactose intolerant or gluten sensitive. Food intolerances or sensitivities can trigger a range of symptoms including bloating, gas, diarrhea, and abdominal pain.
Psychological Stress: Psychological stress has a profound impact on digestive health, mediated through the gut-brain axis. This communication pathway operates in both directions, which means that stress can disrupt normal digestive processes. This can lead to symptoms like irritable bowel syndrome (IBS), heartburn, indigestion, and changes in bowel habits. Chronic psychological stress can change gut motility, increase intestinal permeability (contributing to conditions like “leaky gut”), influence the balance of gut bacteria, and affect the body’s ability to digest food and absorb nutrients effectively. This can result in gastrointestinal discomfort and a range of symptoms such as bloating, pain, diarrhea, or constipation. Managing psychological stress is a major part of addressing various digestive disorders. Techniques such as cognitive-behavioral therapy, mindfulness, relaxation exercises, and regular physical activity can be effective in reducing stress and improving gut health. Additionally, a well-balanced diet, adequate sleep, and social support play important roles in mitigating the effects of psychological stress on the digestive system.
Physiological Stress: Physiological stress can impact the gastrointestinal (GI) tract. This includes not only the intense physical exertion experienced by athletes but also other forms of bodily stress such as surgery, severe illness, trauma, or chronic medical conditions. During these states, the body often redirects blood flow away from the GI tract to prioritize vital organs, leading to a decrease in gut motility and altered digestive function. This redirection can result in a range of digestive symptoms, including nausea, constipation, abdominal pain, and changes in gut microbiota. Dehydration and electrolyte imbalances, common in these conditions, can make GI symptoms worse. In severe cases, such as in critical illness or after major surgery, the integrity of the gut barrier can be compromised, leading to complications like bacterial translocation and systemic inflammation. The body’s response to these physiological stresses often involves the release of stress hormones like cortisol, which can further change digestive processes. Effective management of these challenges involves not only addressing the primary cause of the stress but also ensuring adequate nutrition and hydration, monitoring and managing symptoms, and in some cases, using medications to support gut motility and function.
Infections: Infections in the digestive system can be caused by bacteria, viruses, or parasites, leading to gastroenteritis. Symptoms often include diarrhea, vomiting, and abdominal cramps. Bacterial infections, such as those caused by Helicobacter pylori, can lead to more serious conditions like stomach ulcers and gastritis. These bacteria disrupt the mucous layer that protects the stomach lining, allowing acid to erode the lining and create ulcers. Viral infections, like norovirus or rotavirus, are common causes of acute gastroenteritis, particularly in children. Parasitic infections, although less common in developed countries, can occur through contaminated food or water and lead to symptoms like diarrhea, abdominal pain, and bloating.
Medications: Various medications can impact digestive health, often as side effects. Antibiotics, while crucial for treating bacterial infections, can disrupt the natural balance of the gut microbiota. This disruption can lead to conditions like antibiotic-associated diarrhea or Clostridium difficile (C. diff) infection. Nonsteroidal anti-inflammatory drugs (NSAIDs) and certain pain relievers can irritate the stomach lining, increasing the risk of stomach ulcers and gastritis. These medications can inhibit the production of prostaglandins, substances that protect the stomach lining. Prolonged use of certain drugs, such as proton pump inhibitors (used for acid reflux), can also lead to changes in stomach acidity, potentially affecting the gut microbiome and nutrient absorption. Understanding and managing these side effects, often through dosage adjustments or alternative medications, is crucial, especially for individuals on long-term medication regimens.
Functional Disorders: Conditions like Irritable Bowel Syndrome (IBS) and functional dyspepsia fall under the category of functional gastrointestinal disorders. These conditions usually have symptoms such as abdominal pain, bloating, and altered bowel habits in the case of IBS, or persistent indigestion in the case of functional dyspepsia. Despite their impact on quality of life, these disorders often do not have identifiable structural or biochemical abnormalities as their basis. They are thought to arise from complex interactions between the gut and the brain, known as the gut-brain axis. This interaction includes abnormal gut motility, heightened visceral sensitivity, and psychosocial factors. Treatment often involves a combination of dietary changes, stress management, behavioral therapy, and medications tailored to symptom relief.
Structural Abnormalities: Structural abnormalities in the digestive system, such as hernias, bowel obstructions, or diverticulitis, can lead to major digestive issues. Hernias, which involve the protrusion of an organ through a weak spot in the surrounding muscle or tissue, can cause pain and discomfort, especially when they occur in the abdominal region. Bowel obstructions, resulting from conditions like adhesions, tumors, or strictures, can lead to severe abdominal pain, vomiting, constipation, and bloating. Diverticulitis, inflammation of the diverticula (small pouches in the colon walls), can cause acute pain, fever, and changes in bowel habits. These structural issues often require medical or surgical intervention, depending on their severity and the associated risks. Accurate diagnosis through imaging and other diagnostic tools is essential for effective treatment planning.
Autoimmune Disorders: In autoimmune digestive disorders like Celiac Disease and Inflammatory Bowel Disease (IBD), the body’s immune system mistakenly attacks parts of the digestive system, leading to inflammation and other symptoms. Celiac Disease is triggered by gluten consumption and leads to damage in the small intestine, impairing nutrient absorption and causing symptoms like diarrhea, bloating, and weight loss. IBD, which includes Crohn’s Disease and Ulcerative Colitis, causes chronic inflammation anywhere along the GI tract (in Crohn’s) or specifically in the colon and rectum (in Ulcerative Colitis). Common symptoms include abdominal pain, severe diarrhea, fatigue, weight loss, and sometimes blood in the stool. The exact causes of these autoimmune responses are not fully understood, but they are believed to involve a combination of genetic and environmental factors.
Genetic Factors: Genetics play a role in the susceptibility to various digestive conditions. For instance, certain genetic mutations are linked to a higher risk of developing IBD, gastrointestinal cancers, and liver diseases. In conditions like Crohn’s Disease and Ulcerative Colitis, family history is a known risk factor. Similarly, genetic predispositions can influence the development of colorectal cancer and other gastrointestinal malignancies. Liver diseases like hemochromatosis, where iron accumulates in the body, can also have genetic underpinnings. Understanding these genetic connections helps in early detection and personalized treatment strategies.
Gut Microbiome Imbalance: The gut microbiota, an intricate ecosystem of microorganisms in the digestive system, plays a vital role in overall health, including digestion, nutrient absorption, and immune system function. An imbalance in this microbiome, known as dysbiosis, can disrupt these processes and lead to various digestive issues like inflammatory conditions, and irritable bowel syndrome, and even contribute to the development of obesity and mental health issues. Factors contributing to dysbiosis include poor diet, prolonged use of antibiotics or other medications, and illnesses. Restoring and maintaining a healthy gut microbiome often involves dietary changes to include prebiotic and probiotic foods, and in some cases, may require medical intervention.
Psychological Factors: The gut-brain axis is a complex communication network linking the emotional and cognitive centers of the brain with peripheral intestinal functions. Stress, anxiety, and depression can have an impact on the gut, potentially worsening or even triggering digestive problems such as IBS, heartburn, and stomach ulcers. These psychological factors can affect gut motility and sensitivity, leading to symptoms like pain, bloating, and altered bowel habits. Conversely, issues in the gut can impact mental health, creating a bidirectional relationship. Treatment approaches often include stress management techniques, psychological therapies, and, when necessary, medications to address both digestive and mental health concurrently.
Histamine Intolerance: Histamine intolerance is an under-recognized cause of digestive problems related to the accumulation of histamine and the body’s ability to break it down. Histamine plays a vital role in the body’s immune response, but in excessive amounts, it can lead to symptoms including diarrhea, abdominal pain, bloating, and nausea. In people with histamine intolerance, the enzyme responsible for breaking down histamine in foods – diamine oxidase (DAO) – is either low or not functioning properly. This can lead to a buildup of histamine in the body, triggering an array of digestive and systemic symptoms. Common food sources of histamine include aged cheeses, fermented products, cured meats, and some alcoholic beverages. Diagnosis of histamine intolerance is often challenging due to its overlapping symptoms with other food intolerances and gastrointestinal disorders. Management usually involves avoiding histamine-rich foods and may include supplementation with DAO enzymes to help in histamine breakdown. Identifying and addressing histamine intolerance can significantly improve quality of life for those affected by this condition.
IgG food sensitivities: IgG food sensitivities are increasingly being explored as a potential cause of digestive issues in individuals who don’t find relief from traditional dietary modifications or for whom standard diagnostic tests fail to identify a clear cause. Unlike “true food allergies”, which involve IgE antibodies, IgG food sensitivities are associated with a delayed immune response. The theory is that IgG antibodies react to certain foods, leading to a gradual immune response that can show up as various digestive symptoms, including bloating, gas, abdominal pain, diarrhea, and constipation. These symptoms might arise hours or even days after consuming the triggering food, making it challenging to identify the cause. Testing for IgG food sensitivities often involves blood tests that identify specific foods to which an individual has developed IgG antibodies. However, the clinical significance and interpretation of these tests remain controversial among medical professionals. Some practitioners consider them useful in identifying foods that might be contributing to chronic inflammation and gastrointestinal discomfort, while others question their reliability and relevance due to a lack of consistent scientific evidence supporting their use. For people with persistent, unexplained digestive problems, exploring IgG food sensitivities may offer a way to identify food triggers and tailor a food plan. It should be approached with careful consideration and under the guidance of healthcare professionals experienced with IgG food sensitivity testing. [PMC6074204]
Symptom Overlap
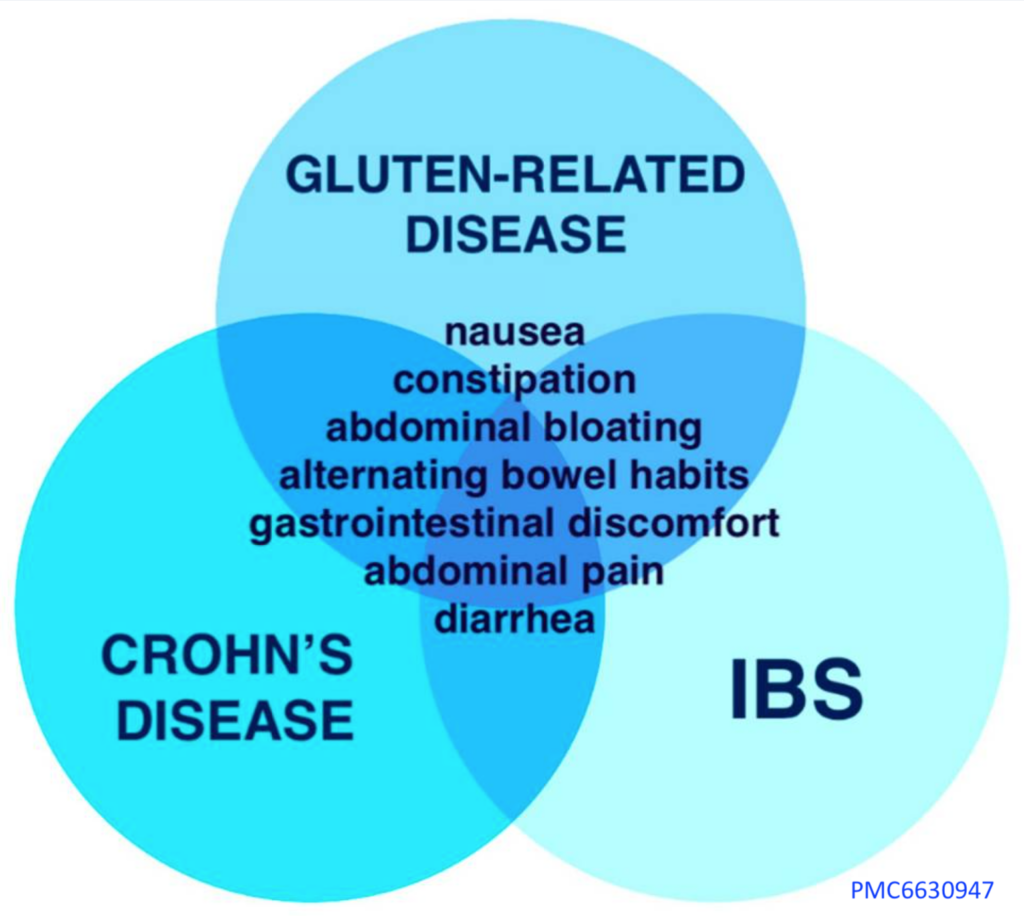
The illustration shows how many different digestive problems can cause identical symptoms.
This leads to a great deal of difficulty in identifying the root cause of digestive symptoms.
What Are Different Types of Digestive Problems?
Gastroesophageal Reflux Disease (GERD): GERD is a condition where stomach acid frequently flows back into the esophagus, the tube connecting the mouth and stomach, leading to irritation. Common symptoms include heartburn, regurgitation of food or sour liquid, and difficulty swallowing. It’s often seen in individuals who are obese, pregnant, smokers, or those with a hiatal hernia. Certain medications can also increase the risk. Treatment typically focuses on lifestyle modifications like diet changes, weight loss, and avoiding known triggers such as spicy foods, caffeine, and alcohol. For more severe cases, medications like antacids, H2 blockers, and proton pump inhibitors may be necessary.
Irritable Bowel Syndrome (IBS): IBS affects the large intestine and is characterized by symptoms like cramping, abdominal pain, bloating, gas, alternating diarrhea, and constipation. The exact cause of IBS remains unknown, but it may involve a combination of intestinal muscle contractions, nervous system abnormalities, inflammation following an infection, changes in gut bacteria, and other factors. Treatment focuses on relieving these symptoms and often includes dietary adjustments, stress management, and medications such as fiber supplements, laxatives, anti-diarrheal drugs, anticholinergics, and pain relievers.
Inflammatory Bowel Disease: Inflammatory Bowel Disease (IBD) is an autoimmune disorder that encompasses Crohn’s Disease and Ulcerative Colitis, both involving chronic inflammation of the gastrointestinal tract. As an autoimmune condition, IBD occurs when the body’s immune system mistakenly attacks the digestive tract, leading to persistent inflammation. This abnormal immune response is thought to be triggered by a combination of genetic predisposition and environmental factors. Crohn’s Disease can affect any part of the GI tract, often impacting the end of the small bowel and the beginning of the colon, while Ulcerative Colitis usually affects only the colon and rectum. Common symptoms include severe diarrhea, abdominal pain, weight loss, and fatigue. The management of IBD focuses on controlling the immune response to reduce inflammation, alleviate symptoms, and prevent flare-ups. This often involves medication, dietary adjustments, and in some cases, surgery. Given its chronic nature and impact on quality of life, comprehensive care, including psychological support, is crucial for individuals living with IBD.
Gastritis: Gastritis is the inflammation of the stomach lining, often resulting from factors like Helicobacter pylori infection, regular NSAID use, excessive alcohol consumption, stress, or autoimmune conditions. Symptoms include nausea, vomiting, a feeling of fullness in the upper abdomen after eating, and indigestion. Gastritis can be acute or chronic, with chronic gastritis potentially lasting for years if untreated. Treatments generally involve using antacids and other medications to reduce stomach acid, which helps alleviate symptoms and promote healing of the stomach lining.
Peptic Ulcers: Peptic ulcers are sores that develop on the lining of the stomach, upper small intestine, or esophagus. Commonly caused by Helicobacter pylori infection and prolonged NSAID use, they present symptoms like burning stomach pain, bloating, heartburn, intolerance to fatty foods, nausea, and in severe cases, vomiting of blood or presence of blood in stools. Complications can include internal bleeding, infection, and obstruction. Treatment typically involves medications to decrease stomach acid production and antibiotics to treat Helicobacter pylori infection, if present.
Celiac Disease: Celiac disease is a serious autoimmune disorder triggered by consuming gluten, a protein found in wheat, barley, and rye. In individuals with celiac disease, ingestion of gluten leads to an immune response that damages the lining of the small intestine. This damage impairs nutrient absorption and can lead to a variety of symptoms including diarrhea, bloating, gas, fatigue, low blood count (anemia), and osteoporosis. Some individuals may have no gastrointestinal symptoms but experience other signs like anemia, irritability, or depression. The only effective treatment for celiac disease is a strict gluten-free diet, which helps heal the intestinal damage and prevent further complications. Adhering to this diet can be challenging as gluten is present in many foods, but it is crucial for managing the condition.
Gallstones: Gallstones are hard deposits that form in the gallbladder, a small organ beneath the liver. These stones can range in size and are composed primarily of hardened cholesterol or bilirubin. They can cause pain in the upper right abdomen, particularly after eating fatty foods. This pain can be severe and may lead to nausea or vomiting. Gallstones can also obstruct the flow of bile from the gallbladder, leading to a condition known as cholecystitis, an inflammation of the gallbladder. Treatment options for gallstones include surgical removal of the gallbladder (cholecystectomy), medications to dissolve the stones, or non-surgical procedures to break them down.
Pancreatitis: Pancreatitis is the inflammation of the pancreas, an organ that lies behind the lower part of the stomach. This condition can manifest as acute pancreatitis, which is sudden and severe, or chronic pancreatitis, which is persistent over time. Causes of pancreatitis include gallstones, alcoholism, certain medications, and abdominal surgery. Symptoms include intense abdominal pain, nausea, vomiting, fever, and rapid pulse. Acute pancreatitis can be a life-threatening condition requiring immediate medical attention. Chronic pancreatitis, while less severe initially, can lead to long-term complications like malnutrition, diabetes, and an increased risk of pancreatic cancer. Treatment typically involves hospitalization with supportive care for acute attacks, and lifestyle changes, pain management, and enzyme supplements for chronic cases.
Diverticulitis: Diverticulitis occurs when small pouches, known as diverticula, that have formed in the walls of the colon become inflamed or infected. These pouches are common, especially after age 40, and do not cause problems in most cases. However, if they become inflamed or infected, symptoms like pain in the lower left side of the abdomen, fever, nausea, and a change in bowel habits can occur. Causes of diverticulitis are not precisely understood but are believed to include factors like a low-fiber diet, obesity, and lack of regular physical activity. Treatment depends on the severity of the condition but can range from dietary changes and antibiotics to surgical intervention in severe or recurrent cases.
Gastroenteritis: Commonly known as stomach flu, gastroenteritis is an inflammation of the lining of the stomach and intestines, typically resulting from an infectious cause, such as a virus or bacteria. It’s characterized by symptoms like diarrhea, abdominal cramps, nausea, vomiting, and sometimes fever or headache. The infection can be spread through contaminated food or water, or close contact with an infected person. The primary concern with gastroenteritis is dehydration, especially in young children and older adults. Treatment focuses on staying hydrated and managing symptoms. In most cases, gastroenteritis resolves without specific medication, but severe cases, particularly those caused by bacteria, may require antibiotics. Preventive measures include good hygiene practices and proper food handling.
Liver Problems: Bowel dysfunction can often be a complication of liver problems, such as cirrhosis or alcoholic hepatitis, due to the liver’s pivotal role in digestion and toxin removal. In conditions like cirrhosis, where the liver is damaged and scarred, its ability to produce bile – essential for fat digestion – is impaired, leading to malabsorption and diarrhea. This compromised bile production can also result in steatorrhea, where fats are not properly digested, causing fatty, loose stools. The liver’s lack of capacity to detoxify can also impact the gut microbiome, possibly leading to bacterial overgrowth. This can cause changes in bowel function, leading to as bloating, discomfort, and irregular bowel movements.
Constipation: Constipation is a common digestive issue where an individual experiences difficulty in passing stools or has infrequent bowel movements. It often results from dietary factors, such as insufficient fiber intake, inadequate fluid intake, or a sudden change in diet. Lifestyle factors like lack of physical activity, certain medications (such as painkillers or antidepressants), and various medical conditions (like diabetes or thyroid disorders) can also contribute to constipation. Symptoms include passing fewer than three stools a week, straining to have bowel movements, hard or lumpy stools, and a feeling of incomplete evacuation. Management of constipation typically involves dietary and lifestyle modifications, including increased fiber and fluid intake and regular exercise. In some cases, over-the-counter laxatives may be used, but they should be taken with caution and under medical advice.
Diarrhea: Diarrhea is characterized by frequent, loose, or watery bowel movements and is a common issue that affects nearly everyone at some point. It can be caused by a variety of factors, including infections (such as those from certain bacteria, viruses, or parasites), certain medications (like antibiotics), and chronic diseases (such as Crohn’s disease or irritable bowel syndrome). Symptoms accompanying diarrhea may include abdominal cramps, bloating, and an urgent need to use the bathroom. While it usually resolves on its own within a few days, diarrhea can lead to dehydration, particularly in young children and older adults. Treatment primarily involves rehydration through drinking fluids or taking oral rehydration solutions. If diarrhea is due to a bacterial infection or a certain medical condition, further medical treatment may be required. Probiotics and dietary adjustments can also be helpful in managing and preventing recurrent episodes.
Diarrhea Caused By Constipation: Diarrhea that is seemingly paradoxically caused by constipation is a condition known as “overflow diarrhea” or “paradoxical diarrhea.” It occurs when prolonged constipation leads to an impaction, a condition where a hard mass of stool becomes stuck in the colon. This impaction blocks the colon, preventing normal passage of stool. However, the body continues to produce waste, and over time, liquid stool can start to seep around the impacted mass. This liquid stool can then pass through the rectum, presenting as diarrhea. Symptoms of this condition may include a combination of constipation and diarrhea, abdominal pain, bloating, and a feeling of incomplete evacuation. Overflow diarrhea is often confusing and distressing for the individual experiencing it, as it combines symptoms of both constipation and diarrhea. It’s important to address this condition promptly as it can indicate severe constipation and may require medical intervention to remove the impaction and restore normal bowel function. Treatment may involve the use of laxatives, enemas, manual removal of stool, and changes in diet and lifestyle to prevent recurrence.

When you purchase linked products presented on this page, Supplement Sciences, LLC receives affiliate fees so that our dietitians can continue to create great content.
Thank you for your support!
What Lab Tests Are Useful For Diagnosing Digestive Problems?
Blood Tests For Bleeding or Infection:
- Complete Blood Count (CBC): Used to check for anemia, infection, and other blood-related issues. Anemia could be indicative of chronic gastrointestinal bleeding, common in conditions like inflammatory bowel disease (IBD) or peptic ulcers.
Standard Diagnostic Stool Tests: Stool tests are a fundamental component of diagnosing various gastrointestinal conditions. They involve analyzing a sample of stool to detect abnormalities that can indicate specific health issues:
- Presence of Blood: This can signal bleeding in the gastrointestinal tract, which might be due to conditions like hemorrhoids, inflammatory bowel disease (IBD), or gastrointestinal cancers.
- Fat in Stool (Qualitative or Quantitative Stool Fat): High levels of fat in stool (steatorrhea) can indicate malabsorption disorders, where the body is unable to adequately absorb fat and other nutrients from the diet. Conditions like chronic pancreatitis, celiac disease, or cystic fibrosis can lead to malabsorption.
- Parasites, Bacteria, or Viruses: Detecting pathogens in stool can diagnose infections. These include bacterial gastroenteritis, parasitic infections like giardiasis, or viral infections like norovirus or rotavirus. Specific tests, such as culture tests, ova and parasite (O&P) exams, or PCR tests, are used depending on the suspected organism.
- Stool Culture: Used to identify bacteria that might be causing an infection. It’s particularly useful when a patient has persistent diarrhea.
Blood Tests For Inflammation: Both ESR and CRP are nonspecific tests and can be elevated in many inflammatory conditions, including IBD.
- Erythrocyte Sedimentation Rate (ESR): This test measures how quickly erythrocytes (red blood cells) settle at the bottom of a test tube over a specified period. A faster-than-normal rate may indicate inflammation in the body, which is seen in various conditions, including IBD, infections, and autoimmune disorders.
- C-Reactive Protein (CRP): CRP is a protein produced by the liver in response to inflammation. Elevated CRP levels can indicate inflammation due to a variety of causes, including infections and chronic diseases like IBD.
Fecal Calprotectin or Lactoferrin: These are specific tests for inflammation in the intestines. These tests differentiate between different Irritable Bowel Syndrome and Inflammatory Bowel Disease, which can share similar symptoms. High levels of these proteins in stool samples show active inflammation, which is a hallmark of conditions like Crohn’s disease and ulcerative colitis. In contrast, lower levels are more consistent with IBS, which is usually not associated with as much inflammation. Both fecal calprotectin and lactoferrin tests are valuable in guiding the diagnostic process and in monitoring the effectiveness of treatment for conditions like IBD.
- Fecal Calprotectin: This is a protein found in white blood cells and is a marker of inflammation in the gastrointestinal tract. Elevated levels of fecal calprotectin can suggest active inflammation, as seen in IBD. It’s particularly useful in distinguishing IBD from irritable bowel syndrome (IBS), as IBS does not typically cause increased levels of calprotectin.
- Fecal Lactoferrin: Similar to calprotectin, lactoferrin is another protein that’s released from white blood cells during inflammation. It is also used to differentiate between IBD and IBS and can help in monitoring disease activity in known cases of IBD.
Celiac Disease Antibody Blood Tests: These tests are valuable diagnostic tools in gastroenterology as they involve the detection of specific antibodies in the blood for Celiac Disease. These tests are particularly valuable as they are less invasive than procedures like biopsies and can provide quick and essential diagnostic information.
- Tissue Transglutaminase Antibodies (tTG-IgA): This test is crucial in the diagnosis of celiac disease. Celiac disease is an autoimmune disorder where eating gluten leads to damage in the small intestine. The presence of tTG-IgA antibodies is highly suggestive of celiac disease, especially when correlated with clinical symptoms and other diagnostic criteria.
Breath Tests: Breath tests are non-invasive tests used for diagnosing certain digestive disorders:
- Lactose Intolerance Test: This test measures hydrogen in the breath after consuming a lactose-containing drink. Excessive hydrogen production indicates that lactose is not properly digested, suggesting lactose intolerance.
- Small Intestinal Bacterial Overgrowth Test: Similar in methodology, this test can detect bacterial overgrowth in the small intestine. Patients drink a sugar solution, and the test measures hydrogen and methane gases produced by bacteria in the intestine.
Upper Endoscopy or Colonoscopy Biopsy Tests: These are critical diagnostic tools in gastroenterology:
- During an Upper Endoscopy or Colonoscopy: Small tissue samples (biopsies) can be taken from the lining of the GI tract. This is essential for diagnosing various conditions, including celiac disease, where biopsy samples might show characteristic damage to the small intestine’s lining; inflammatory bowel diseases like Crohn’s disease and ulcerative colitis; and various gastrointestinal cancers.
- Histological Examination: The tissue samples are examined under a microscope for abnormalities, providing valuable information about the presence and extent of disease.
Pancreatic Function Tests: These tests are used to assess the pancreas’s ability to produce digestive enzymes:
- Tests for Exocrine Pancreatic Insufficiency (EPI): These might include fecal elastase or fecal fat tests, which measure enzyme levels or fat content in the stool. Diagnosing Exocrine Pancreatic Insufficiency (EPI) typically involves specialized tests that focus on pancreatic function. The fecal elastase test is a primary diagnostic tool, analyzing stool samples for elastase, an enzyme produced by the pancreas. Low levels of fecal elastase are indicative of EPI, suggesting a deficiency in pancreatic enzyme production. Blood tests can also be used to assess related complications and nutritional deficiencies that may arise from EPI, such as vitamins A, D, E, and K levels, and to check for associated conditions like diabetes. In some cases, direct pancreatic function tests, like the Secretin Stimulation Test, might be employed for more detailed assessment. This combination of stool and blood tests, along with a clinical evaluation of symptoms like weight loss, diarrhea, and abdominal discomfort, aids in the accurate diagnosis and subsequent management of EPI.
- Chronic Pancreatitis Diagnosis: In chronic pancreatitis, the pancreas loses its ability to produce enough enzymes, which can lead to malabsorption and digestive symptoms. The fecal elastase test, which measures pancreatic enzyme levels in the stool, is commonly used to indicate pancreatic insufficiency often seen in chronic pancreatitis. Additionally, blood tests, though not diagnostic on their own, help evaluate complications or related factors by measuring pancreatic enzymes like amylase and lipase, and assessing for diabetes, a frequent complication of chronic pancreatitis. These tests, combined with an evaluation of symptoms such as abdominal pain and weight loss, contribute to the diagnosis, especially when risk factors like alcohol use are present. This streamlined approach, focusing on stool and blood tests, plays a key role in diagnosing and managing chronic pancreatitis effectively.
Stool Microbiome Testing
Once conventional tests have been conducted to rule out conditions like celiac disease, inflammatory bowel disease (IBD), and pancreatic issues, the GI-effects or similar stool microbiome tests can provide valuable additional insights into an individual’s gut health, particularly when symptoms persist or when the cause of gastrointestinal discomfort remains unclear.
After ruling out these specific conditions, the focus often shifts to understanding the broader ecological landscape of the gut. This is where stool microbiome tests come into play. They offer a comprehensive analysis of the gut’s microbial environment, shedding light on aspects that are not typically covered by standard tests. For instance, they can identify subtle imbalances in the gut flora, such as a decrease in beneficial bacteria or an overgrowth of potentially harmful microorganisms. Such dysbiosis can contribute to a range of symptoms, including bloating, irregular bowel movements, and abdominal discomfort.
These tests also measure markers of gut inflammation and digestive function. Even in the absence of conditions like IBD, low-level inflammation can still occur and can be indicative of food sensitivities, ongoing low-grade infections, or other functional gastrointestinal disorders. Additionally, they can assess the efficiency of digestive processes, providing information on aspects like enzyme activity, bile acid metabolism, and fat absorption, which can be subtly affected even when pancreatic function is deemed normal.
Moreover, the insights gained from stool microbiome tests can guide targeted therapeutic interventions. For example, if a significant imbalance in the gut flora is detected, a healthcare provider may recommend a tailored probiotic regimen, specific dietary changes, or even prebiotic supplements to restore a healthy microbiome balance. This personalized approach can be particularly beneficial for individuals with gastrointestinal symptoms that have not been adequately explained or resolved by standard testing and treatment protocols.

When you purchase linked products presented on this page, Supplement Sciences, LLC receives affiliate fees so that our dietitians can continue to create great content.
Thank you for your support!
Order Supplement For Digestive Health
Why Professionals Choose the Fullscript Formulary
Your health is on the line. Health professionals know that many other online and retail options set a very low bar for quality–sometimes amazingly low. The Fullscript formulary is the most secure online source for the highest quality brands securely sourced to assure freshness and purity. Here’s what makes Fullscript the best:
- Meticulous vetting of brand quality. Health professionals trust Fullscript to continuously monitor the quality of each item on the platform. Other retailers operate with profit as their highest or only motive when choosing brands. Fullscript cares only about quality and reliability. Unlike discount stores, large online marketplaces, and other retailers you won’t find ingredients sourced from China or other questionable locations or companies.
- Always 20% Discount off the manufacturer’s retail price. When you follow any link from Supplement-Sciences.com, you will automatically get 20% off the retail price.
- Free shipping over $50.
- Freshness. Fullscript prioritizes freshness over bulk buying even if it means an increased risk of briefly being out of stock.
- Top quality phone and online support. When you call, knowledgeable humans at Fullscript answer your questions.
- How It Works:
- Easy Sign-up & No Spam Email: Click the “View Product” button below to be taken to Fullscript’s login page where you can quickly create your secure account with just your name, email, and phone number. Then you will be taken directly to the product page.
- Wide variety of supplement options: Once you sign in to your account, you are not limited to the products listed below. You will see similar items listed at the bottom of each product page on Fullscript.
- Search For What You Want: Once inside Fullscript, you can search for the exact brands and products you want from their wide selection of quality brands.
Food First!
Although this article discusses supplements in detail, don’t forget that we are absolutely committed to the “Food First” approach to nutrition. When it comes to your health, the totality of your eating habits far surpasses the impact of individual nutrients or any single supplement you consume. Even though this article doesn’t delve into the broader picture of your overall diet, it’s crucial to keep this element at the forefront of our minds. Your food needs to provide all the vitamins, minerals, fiber, and phytochemicals to nourish your body systems down to the cellular level.
Food choices, rather than supplements, are the most critical factors for a healthy gut microbiome. These trillions of tiny inhabitants in your gut affect your brain waves; they orchestrate your immune system. They possess the power to create molecules that can switch genes on or off and are even capable of synthesizing neurotransmitters. Opting for organic foods and steering clear of plastic packaging (including those labeled BPA-free) is a smart move to limit toxin exposure. The sum of all these parts leads to a powerful conclusion: the ultimate key to your health lies in the quality and balance of the food you consume. Supplements are secondary.
To Sum It Up
Digestive complaints can stem from a variety of causes, ranging from too little fiber and to medical conditions like celiac, IBD, IBS, or others. Factors like poor food choices, lack of physical activity, and high stress levels significantly impact digestive health, often leading to issues like constipation, diarrhea, and heartburn. Medical conditions such as Irritable Bowel Syndrome, Inflammatory Bowel Disease, and gastroesophageal reflux disease are also common culprits. Additionally, food intolerances, allergies, and infections play a significant role in digestive discomfort. Pinpointing the underlying cause is key to finding relief. See a physician to rule out some of the causes of digestive complaints, and consider some of the functional tests to further guide your strategy for achieving gut health.
This Article is Not a Substitute for Medical Advice
Dietary supplements are not designed to diagnose, treat, cure, or prevent any disease. The Supplement Sciences website seeks to provide comprehensive access to the most relevant supplement information along with convenient online ordering. We do not provide medical advice and cannot guarantee that every product suggested is completely without risk. Since each person is unique in their health history and medication use, it is important to discuss supplements with your personal physician. Specifically, pregnant women and individuals being treated for cancer or liver or kidney problems must consult their physician about every nutritional supplement they plan to take. People taking medications for the treatment of HIV or with a history of organ transplant must not take supplements without consulting with their physician.

 Scan Me!
Scan Me!

